The definition of a war according to Frankel and Joseph (2025) in Britannica is as follows :
“ War, in the popular sense, refers to a conflict between political groups involving hostilities of considerable duration and magnitude.”More often than not, the physical effects of war often takes the headlines in news reports, media, and public discourses, thereby leading to the overlooking and under-recognition of the psychological aftermath and impact on individuals.
In the light of the considerable duration and magnitude of war, along with the ongoing situation of India - Pakistan the impact of such turbulent war situations and environments on the mental health of both, the military veterans on the borders as well as of the civilians of both countries is a critical area for understanding the devastating consequences of war on the mental health of all those involved.
As shown in the statistics above, conflict situations and wars have an extreme tendency to have an impact on an individual's mental health.
This blog post focuses on some of the mental health impacts of war on both parties impacted. It also examines the psychological interventions that promote long-term psychological health, healing, and effective coping, while addressing some of the challenges encountered when treating the war-affected populations.
Impact/effects of war on civilians and military veterans- PTSD
- Anxiety
- Depression
- Unhealthy Coping Mechanisms and Substance Use
- Distress due to Media Exposure
The brave men and women, who serve their country and as a result, live constantly with the war inside them, exist in a world of chaos. But the turmoil they experience isn't who they are; the PTSD invades their minds and bodies.
? Robert Koger, Death's RevengeThe quote captures the impact of war and its relationship with PTSD in military veterans.Both military veterans and civilians frequently experience the symptoms of Post-Traumatic Stress Disorder (PTSD), marked by intrusive memories and nightmares as well as intense flashbacks of the war. Research has shown that 9 - 25% of war veterans develop PTSD symptoms.
It is to be noted that PTSD is a multifaceted condition which can be typically categorized into four main clusters of symptoms:
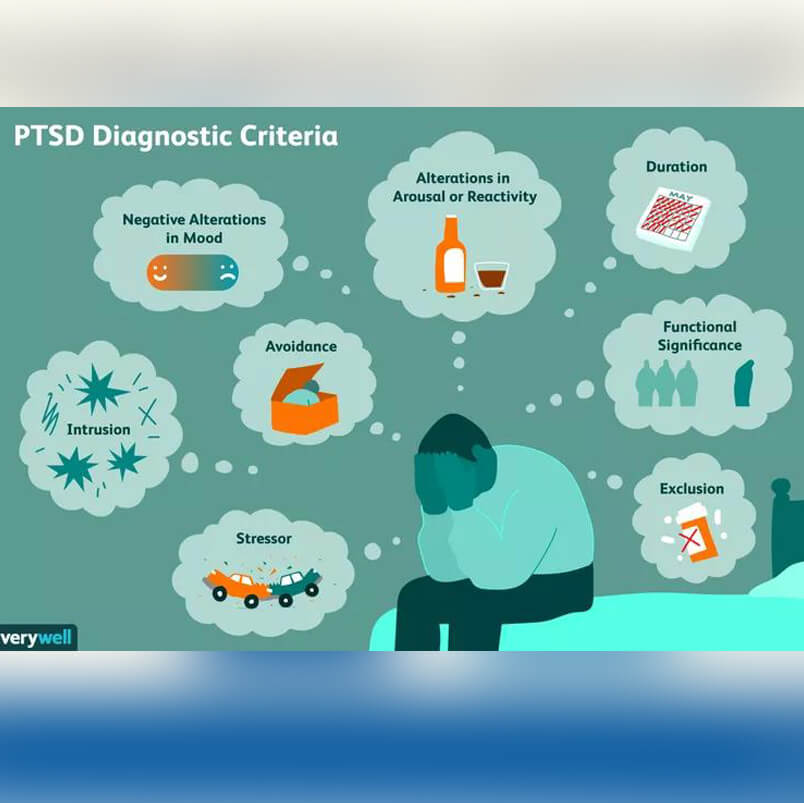
Avoidance: Involves avoiding the reminders of trauma experienced.
Negative alterations in cognition and mood: Emotional numbness, hopelessness
Arousal and reactivity: Irritability, hypervigilance
Intrusion: Flashbacks and distressing dreams These symptoms demonstrate the complex, intrusive, and devastating nature of the disorder, considerably affecting the mental health of those affected.
The environment of war and conflict creates a persistent sense of uncertainty, which often results in a heightened sense of anxiety, not only during the war but even after it has ended. This constant state of apprehension impacts both civilians and veterans alike, leaving them in a constant state of fear regarding a potential recurrence.
Loss, destruction, as well as exposure to prolonged periods of chaos, often linked to the uncertain environments of war, frequently leads them to develop symptoms of depression. The trauma associated with exposure to the events of war leads to feelings of helplessness, hopelessness, as well as a diminished sense of self-worth, which are commonly associated with depression. Civilians and veterans who witness the death of their loved ones might also suffer from “Survivor's Guilt” – an emotional response marked by feelings of guilt for surviving, often contributing to the occurrence of deeper emotional overwhelm and intense depressive episodes.
The emotional burden, coupled with inadequate access to professional mental health support, leads many individuals, particularly military veterans, to resort to substance use, including alcohol and drugs. This substance dependence often results from the intense need to cope with the resulting negative emotions experienced due to the exposure to war, either through first-hand exposure or through constant viewing of war-related news and media.
The continuous viewing and bombardment of war-related media and news, which are distressing, tends to intensify the emotional overwhelm experienced by the general public. Even though not directly experiencing the war, civilians might experience heightened levels of stress and anxiety through vicarious (observed) trauma.
The psychological impact of war on military veterans and civilians cannot be ignored, given the magnitude of such situations. The continued exposure to elements of war, including violence, loss of lives, displacement of individuals, and other such life-threatening experiences often leads to mental health issues such as post-traumatic stress disorder (PTSD), depression, anxiety and unhealthy coping mechanisms, specifically substance use. Military veterans may find it difficult to reintegrate into civilian life because of their experiences in combat, whereas civilians—particularly families and children, frequently suffer from trauma brought on by seeing the devastation and living through instability. The need for easily accessible mental health care, community healing initiatives, and policy-level interventions targeted at psychological recovery and resilience-building is critical because the effects can last for generations.
A number of psychological interventions can be used for civilians and military veterans alike. For military veterans in particular, the following interventions are used in combat zones:
- Combat and Operational Stress Control (COSC)
- Veteran Mental Health Programs
- Reintegration and Peer Support Systems
The military is seen to use on-site psychological first aid to help soldiers process trauma immediately after exposure to combat. Although COSC can be used as an effective early treatment intervention for the reduction of long-term PTSD risks, it is limited in addressing the deep-seated trauma that manifests later.
The government and organizations of the countries often implement long-term PTSD management programs, including therapy, peer support, and assistance for the reintegration of military veterans into society. Some of the main Veteran Mental Health Programs initiated in India include:
a) The “Tele-MANAS” helpline and cellAt the Armed Forces Medical College in Pune, the Ministry of Defence (MoD) and the Ministry of Health and Family Welfare (MoHFW) have partnered to establish a unique Tele-MANAS cell.
Tele-MANAS helpline is a key element of the National Tele-Mental Health Programme. It offers 24/7 telecounselling services and serves as a special mental health hotline for armed forces personnel.
b) Schemes for Psychological Well-Being of Army personnelThe Indian government has initiated various schemes for improving the psychological conditions of army personnel. These schemes deliver mental health services that are preventive, promotional, and curative via a network of psychiatric hospitals and community education initiatives. High-quality psychiatric care is provided in major Armed Forces hospitals, and qualified military psychological counsellors frequently provide counselling and stress screenings.
In order to provide support in both unit and community settings, Religious Teacher JCOs are also trained to serve as counselors. Lastly, to offer easily accessible psychological support, a phone helpline named "Mansik Sahayata" has been established at every Command Headquarters.
c) Psychological Well-Being Programmes for Navy and Air Force personnelThe Indian government also provides psychological support for navy and air force personnel through initiatives like:
In the Navy, the efforts include providing mental health advisories, training senior non-medical sailors in basic psychological counselling, and having qualified psychological counselors counsel sailors and junior leaders. Stress-relieving events such as Yoga and Art of Living classes are regularly held . A policy on handling behavioral issues and offering counselling services has also been released by the IHQ of the MoD (Navy) – which involves the creation of Station Mental Health Centres, training programs, and mental health education initiatives. Every level of the Naval medical services observes World Mental Health Day on October 10th to increase awareness and support mental health.
Similarly, the Indian Air Force has implemented a variety of programs to support mental health. Trained clinical psychologists offer both individual and family counselling. Officers and airmen can identify early indicators of psychiatric symptoms through a four-day service mentor course, personnel are trained in a 12-week program at Command Hospital Air Force, Bangalore, to serve as service counselors.
Individuals who show signs of mental illness are sent to the closest service hospital for additional treatment and monitoring. At the Air Force Central Medical Establishment in Delhi, a toll-free number, the "Manasik Seva Helpline" (1800-110-080), also operates. Regular lectures about mental health are held to raise awareness, and the DGMS (Air) website has a special section with advice on maintaining mental health.
The use of peer-led counselling and veteran support groups would play a pivotal role in normalizing the experiences of PTSD and reducing the stigma linked to it. While this intervention is beneficial for providing social support to the veterans, peer interventions cannot replace structured clinical therapy for severe and debilitating PTSD cases. An example of such peer support systems is the “Wounded Warrior Project” which focuses primarily on holistic rehabilitation through the means of peer connections, resilience-building as well as therapy.
Some of the therapeutic interventions which can be used for civilians as well as military veterans include:
- Cognitive-Behavioral Therapy (CBT)
- Prolonged Exposure Therapy (PE)
- Eye Movement Desensitization and Reprocessing (EMDR)
- Pharmacotherapy (Medication-Based Treatment)
- Alternative and Holistic Approaches
Cognitive-Behavioral Therapy (CBT) focuses on the identification of negative thought patterns associated with trauma experienced, followed by challenging them. This therapy technique is seen to be highly effective, with studies showing that the use of CBT interventions is seen to reduce PTSD symptoms by 50-80%. However, its effectiveness depends on consistent and long-term engagement from the individual.
Prolonged Exposure Therapy (PE) involves helping the individuals repeatedly relive the traumatic experiences in a controlled environment to reduce the possibility of avoidance and fear responses. This therapeutic intervention is seen to reduce hyperarousal and intrusive thoughts. However, some individuals might find it emotionally overwhelming, as it involves the active confrontation of the distressing experiences.
Recognized as an evidence-based treatment for PTSD by the American Psychological Association (APA), Eye Movement Desensitization and Reprocessing (EMDR) involves the reprocessing of the distressing events through bilateral stimulation, such as eye movements and tapping, whilst recalling traumatic memories. This technique is particularly beneficial for the regulation of emotions. However, it requires skilled therapists and has mixed effectiveness in comparison to CBT.
Pharmacotherapy involves the use of medication to manage the psychological symptoms experienced, either as an independent treatment method or in combination with psychotherapy. Common medications used include Selective Serotonin Reuptake Inhibitors (SSRIs) such as Sertraline and Paroxetine- both of which are FDA-approved medications for PTSD. Additionally, these are also used to treat depression, panic disorder, obsessive-compulsive disorder (OCD), social anxiety and premenstrual dysphoric disorder (PMDD). Prazosin is yet another medication that is often prescribed to manage combat-related nightmares and sleep disturbances.
While pharmacotherapy is seen to be effective in the management of anxiety as well as mood symptoms, there are difficulties in addressing the underlying trauma. Which can be addressed mainly through the means of therapy; the use of medication can be beneficial in further alleviating specific symptoms, such as the nightmares experienced. In addition to this, the use of medication for the alleviation of symptoms of disorders and the associated tendency for increased reliance on the medications further leads to concerns.
The stigma surrounding professional mental health support remains prevalent among a vast majority of military veterans and civilians, leading to hesitation and reluctance in taking traditional therapy. Therefore, in order to alleviate the symptoms of disorders (such as PTSD, depression and anxiety) experienced by them due to the exposure to extreme situations of war, there is an increasing need to delve deeper into alternative and non- traditional therapeutic approaches. The use of such approaches would help ensure lower rates of dropouts from therapy and long-term adherence to these therapeutic techniques. Some of the alternative and holistic approaches that can be employed include :
- Mindfulness-Based Stress Reduction (MBSR), which utilizes meditation and breathing techniques to reduce PTSD symptoms.
- Animal-Assisted Therapy, which involves the utilization of service dogs who are trained to recognize and identify PTSD symptoms.
- Art and Music Therapy, which uses art forms to help with emotional expression, along with stress relief.
These alternative and holistic techniques can be used as complementary treatments, particularly for veterans and civilians who are resistant to traditional therapy due to the stigma or discomfort attached to it.
Challenges in PTSD treatment for veteransThe treatment of PTSD and trauma-related symptoms in military veterans presents several challenges. These include stigma towards mental health treatments, reduced adherence to treatment, restricted access to mental health care-especially in rural areas, as well as the co- occurrence of PTSD with other disorders.
One of the most persistent obstacles faced is the stigma. This challenge can be highlighted through this quote by Joan Beder in Advances in Social Work Practice with the Military:
“According to Hoge and colleagues (2007), the key to reducing stigma is to present mental health care as a routine aspect of health care, similar to getting a checkup or an X-ray. Soldiers need to understand that stress reactions- difficulty sleeping, reliving incidents in your mind, and emotional detachment are common and expected after combat... The soldier should be told that wherever they go, they should remember that what they're feeling is "normal and it's nothing to be ashamed of.”
Many military veterans internalize the traditional view that seeking mental health support is a sign of weakness, making them vulnerable and leading to the fear of being seen as “not man enough to solve their problems” by society. This discourages them from addressing their emotional difficulties, often leading to suppression of emotions and deeper emotional health concerns over time.
Even if they start going for therapy and begin taking professional help for their mental health concerns, they might be doing so either hesitantly or due to the compulsion of their loved ones, including their family and friends. In addition to this, since a part of therapeutic techniques like Exposure Therapy (ET) involves reliving the trauma that they experience, they are more likely to drop out of therapy due to the intensity of the trauma and emotions experienced due to reliving the experience.
Another challenge to treatment is when rural veterans or those outside the military healthcare systems struggle to find and utilize PTSD-specific services. Lastly, the co-occurrence of PTSD with other disorders like substance abuse, depression, or even Traumatic Brain Injury (TBI) further complicates the treatment of the disorder.
ResourcesBefore ending this blog, we would like to provide a few mental health helplines and resources in India which can be utilized in times of need:
- Tele-MANAS (1800-89-14416 or short code 14416) : The national tele-mental health helpline provides 24/7 support through a toll-free number (1800-89-14416 or short code 14416). It also has a special cell dedicated to Armed Forces beneficiaries.
- AASRA Foundation (+91-22-27546669 ; 24x7 Helpline ) : This organization provides tele-counselling services during periods of emotional crisis, mental health concerns and cases of suicidal ideations.
- Manasik Sahayta Helpline (1800-110-080)
- For more all-india and a few state selective helplines: http://healthcollective.in/contact/helplines/
In conclusion, it can be said that, while the physical and visible scars of war are more often drawn to the attention of all, the psychological wounds of war are those which are invisible and penetrate deeper into the fabric of the human mind than can be imagined. The acknowledgment of the pain experienced is the first step towards holistic and deeper healing. Luckily, with the ever-growing recognition and acceptance of mental health as equally important as physical health and its crucial role in holistic recovery from circumstances of extreme intensities such as war, a variety of therapeutic interventions including those which are considered traditional along with those which are alternative and holistic brings a sense of hope and roadways to recovery, thereby assisting individuals (both the veterans and civilians) retrieve their sense of peace and purpose in life.
